Stress urinary incontinence is a condition that affects millions worldwide. More than 60% of women deal with some type of urinary incontinence in their lives. Medical help exists, but only 60% of people ask for it. Many stay silent because they feel embarrassed or afraid of social stigma.
This condition goes beyond personal discomfort. The financial cost is a big deal as it means that Americans spend over $13 billion each year to manage it. The good news is that modern treatments give hope to patients. Surgical options show a soaring win with an 84% success rate that helps improve patients’ daily lives.
Understanding Stress Incontinence Basics
Stress incontinence happens when sudden pressure on the bladder leads to unexpected urine leakage. We noticed this condition develops as two muscle groups get weaker: the pelvic floor muscles that hold up the bladder and the urinary sphincter that keeps urine in check.
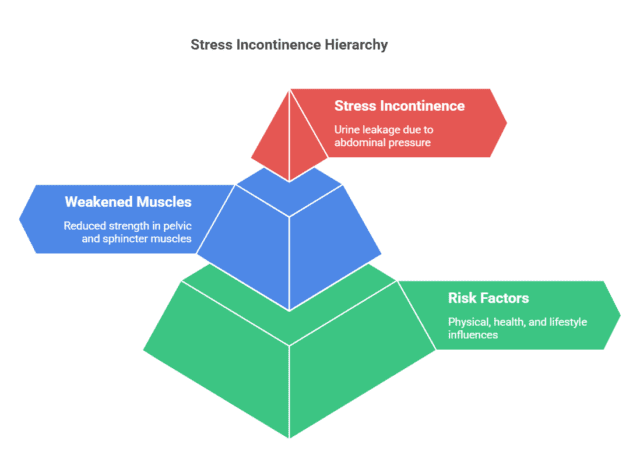
What causes stress incontinence?
The mechanisms behind stress incontinence start with weakened support structures around the urethra. These weakened muscles can’t hold back urine during activities that put pressure on your abdomen. Your sphincter muscle inside the urethra opens briefly under pressure, and that’s what causes the leakage.
Common risk factors
Here’s what can lead to stress incontinence:
- Physical changes: Pregnancy, childbirth (especially vaginal delivery), and menopause
- Health conditions: Chronic coughing, diabetes, and nerve injuries to the pelvis
- Lifestyle factors: Extra weight puts more pressure on your bladder, while smoking bumps up the risk by 1.8 to 2.92 times
Early warning signs
Symptoms vary by a lot from person to person. Mild cases usually show up as small drops of urine that leak out during coughing or laughing. More severe cases might lead to bigger leaks, even with simple movements like standing up or bending down. On top of that, some people notice leaks during intimate moments.
This condition shows up twice as much in people assigned female at birth compared to those assigned male at birth. About 50% of women over 65 deal with stress urinary incontinence. Your chances of getting it go up with age, but that doesn’t mean it’s a normal part of getting older.
Getting the Right Diagnosis
An accurate diagnosis creates the foundation for stress incontinence treatment that works. Healthcare providers use a systematic process to determine the specific type and severity of the condition.
Original medical assessment
The diagnostic process starts with a full medical history review. Healthcare providers ask patients to keep a bladder diary for 3-4 days. The diary tracks fluid intake, urination frequency, and leakage episodes. This detailed record helps spot patterns and triggers of incontinence.
The physical examination focuses on the urinary system. The process includes a pelvic examination. This checks pelvic floor muscle strength and looks for potential organ prolapse. Doctors often use a cough stress test. Patients cough with a full bladder to check for any urine leakage.
The core diagnostic tests
After the first assessment, healthcare providers might recommend several specialized tests:
- Urinalysis: Screens for infections, blood, or other abnormalities that might contribute to symptoms
- Post-void Residual (PVR) Test: Measures remaining urine after bladder emptying through ultrasound or catheterization
- Pad Test: Involves wearing pre-weighed absorbent pads to measure urine loss volume
- Urodynamic Testing: Evaluates bladder and urethral pressures during filling and emptying
These simple tests might show complicated stress incontinence or other concerns. Some cases need a cystoscopy. This test uses a thin tube with a camera to look at the bladder and urinary tract structure.
Treatment Options for Stress Incontinence
Medical science today provides multiple ways to treat stress incontinence, from basic therapies to surgery.
Non-surgical treatments
Healthcare providers recommend starting with basic approaches before considering surgery. Regular practice of pelvic floor exercises (Kegels) shows noticeable improvement in symptoms within 4-6 weeks. Vaginal pessaries are a great way to get bladder and urethral support for patients who want alternatives to surgery.
Several other non-surgical options work well:
- Bladder training through timed voiding
- Vaginal estrogen creams for post-menopausal women
- Lifestyle modifications, including weight management
- Specialized pelvic floor physical therapy with biofeedback
Surgical procedures
Patients need surgical intervention when basic treatments don’t work. The midurethral sling procedure, developed in 1995, remains the most common surgical treatment. This procedure helps 85-90% of patients see substantial improvement. Surgeons usually recommend one of three approaches:
The retropubic sling procedure needs small incisions above the pubic bone, while the transobturator approach goes through groin muscles. The single-incision mini procedure serves as a minimally invasive option for simpler cases.
Recovery timeline
Recovery after surgery depends on the procedure type. Patients can resume their normal activities within 2-6 weeks. They should avoid heavy lifting and strenuous activities during recovery. The procedure’s success rates stay strong, as 80% of women report satisfaction even after 10 years.
Daily Management Strategies
A detailed approach combines targeted exercises, lifestyle changes, and supportive products to manage symptoms.
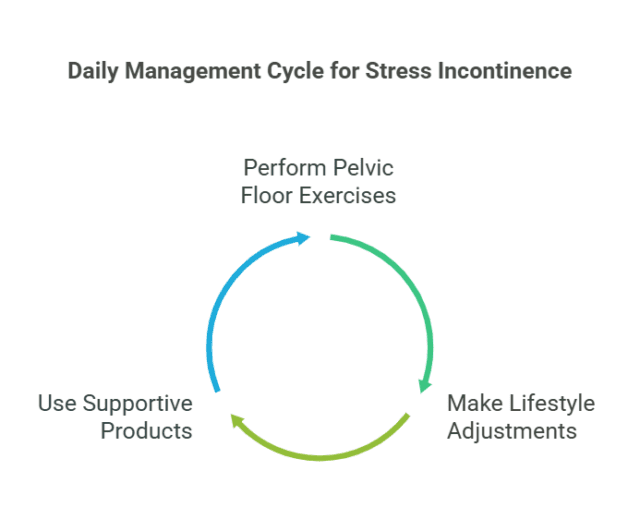
1.Pelvic floor exercises
Pelvic floor muscle training, also known as Kegel exercises, delivers remarkable results when done right. These exercises build strength in muscles that support the bladder and urethra. Studies show an 80% improvement in symptoms. Here’s how to do these exercises:
- Contract the pelvic muscles for 5 seconds
- Relax for an equal count
- Repeat 10-15 times, three times daily
Patients should feel a slight pulling sensation in the pelvic region right away. Notwithstanding that, consistent practice takes 4-6 weeks to show real improvements.
2.Lifestyle adjustments
Several lifestyle changes make a big difference in managing stress incontinence. We focused on maintaining proper fluid intake of 2-2.5 liters daily to prevent bladder irritation. Avoiding bladder irritants brings benefits – these include caffeine, alcohol, and high-citrus content beverages.
Weight management is significant since studies reveal a 20-70% higher risk of urinary incontinence with every five-point increase in BMI. A regular toileting schedule, usually every 2-3 hours throughout the day, helps prevent unexpected leakage.
3.Helpful products and devices
Products of all types help with daily management. Vaginal pessaries, shaped like rings with two bumps, give vital support to the urethra. Absorbent pads and protective underwear offer discrete solutions that match different severity levels.
Biofeedback devices improve exercise results by showing visual feedback about muscle contractions.
Expert Care for Stress Incontinence in Delhi
Epitome hospital stands out as the best stress incontinence hospital in Delhi, offering cutting-edge treatments for this challenging condition. Our team of expert urologists and kidney specialists in Delhi are dedicated to providing the best stress incontinence treatment in Delhi. At Epitome hospitals, we offer advanced treatment options, including state-of-the-art diagnostic tools, personalized pelvic floor therapy, and minimally invasive surgical procedures when necessary.
Our experienced medical staff specializes in tailoring treatment plans to each patient’s unique needs, ensuring optimal outcomes. We emphasize the importance of early intervention, as timely treatment can significantly improve success rates and prevent complications.
By choosing Epitome hospitals for stress incontinence care, patients can expect comprehensive support, from initial diagnosis to long-term management, helping them regain confidence and improve their quality of life.
Conclusion
In conclusion, overcoming stress incontinence requires a comprehensive approach that begins with an accurate diagnosis and is followed by personalized treatment plans.
For the best stress incontinence treatment in Delhi, Epitome hospital offer cutting-edge solutions. With positive success rates, patients can find relief through customized treatment plans. Early intervention and proper diagnosis are crucial for optimal outcomes. Epitome hospital provides the best stress incontinence treatment in Delhi, combining medical expertise with pelvic floor exercises and lifestyle modifications.
Book your appointment at Epitome Hospitals today and take the first step towards effective stress incontinence treatment for a healthier, more confident you!
FAQs
Q1. What are the most common surgical options for stress incontinence?
The most common surgical treatment for stress incontinence is the midurethral sling procedure, which has an 85-90% success rate. There are three main approaches: the retropubic sling, the transobturator approach, and the single-incision mini procedure for less complex cases.
Q2. How long does it typically take to recover from stress incontinence surgery?
Recovery time varies depending on the specific procedure, but most patients can return to regular activities within 2-6 weeks after surgery. It’s important to avoid strenuous activities and heavy lifting during the healing process.
Q3. Are there any non-surgical treatments available for stress incontinence?
Yes, there are several non-surgical treatments for stress incontinence. These include pelvic floor exercises, bladder training, vaginal pessaries, lifestyle modifications like weight management, and specialized pelvic floor physical therapy with biofeedback.
Q4. How Can I reverse stress incontinence?
To reverse stress incontinence, focus on strengthening your pelvic floor muscles with Kegel exercises. Maintain a healthy weight and avoid activities that put excessive pressure on your bladder. Consulting a healthcare provider can help guide you to the best treatment options.

